QUESTION NO 1
1) pt presented vth unable to move his rt upperlimb followed by recurrent episodes of rt sided focal seziures. risk factors in him are alcoholic, smoker, diabetic,on presentation BP was high(170/100mmhg).
According to h/o pt might be having cerebrovascular event follwed by focal seziures.
Anatomical location could be
?frontal lobe involvement ( imp for cognitive functions and control of voluntary movements),
? parietal lobe (it processes information about movement)
could be? anterior circulation stroke.
2) sub cortical infract -
occur in the supplying area of a single, deep perforating brain artery and are mostly felt to be a consequence of cerebral small-vessel disease (CSVD).
Cortical brain infarcts - infarcts involving cortical gray matter, but may differ considerably in size. ... Small cortical infarcts were mainly localized in external watershed areas, whereas large cortical infarcts were localized primarily in large arterial territories.
3) Cerebrovascular diseases, including stroke, are viewed as the most common cause of epilepsy in the elderly population, accounting for 30%-50% of the newly diagnosed cases of epilepsy cases in this age group.
Post-stroke seizures (PSS) have been classified as occurring immediately before, immediately after (24 hours), or of early or late onset. Early-onset seizures are considered to be provoked seizures, which occurred within 1 week or 2 weeks after stroke and caused by the acute metabolic and physiological derangement associated with acute infarction. Late-onset seizures after 2 weeks of stroke are considered to be unprovoked seizures that originate from the areas of partially injured brain where neuronal networks have undergone anatomical and physiological alterations, predisposing them to hyperexcitability and synchronization .
PATHOPHYSIOLOGY:
Neurotransmitter amino acids play an important role in the pathogenesis and development of epilepsy [. Increased concentration of the excitatory neurotransmitter glutamate (Glu), the disturbance of electrolyte balance, the destruction of phospholipid membranes, and the secretion of free fatty acids have been documented in the penumbral areas in the acute post-ischemic stroke phase.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5771387/
4) in some of the ecg shows sinus tachycardia vth vpc's vth leftaxis deviation.i think pt doesn't need anticoagulation.
5) In elderly pts complex partial seziures vthout sec generalization are more common.
Antiepileptic drugs (AEDs) with fewer adverse effects, including cognitive effects, and AEDs without significant pharmacokinetic drug interactions are needed
as LEVIPILL has high efficacy,no drug interactions.no cognitive effects,broad spectrum it is useful.pt is having recurrent episodes of focal seziures levipill dose was inc. but dose adjustment has to be made according to renal clearence.pt is still having seziure episode tab carbamazepine was useful high efficacy.
as pt gfr was reduced levipill dose has to be tappered and pt to be kept on tab carbamazepine.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6706648/.
QUESTION NO 2
1)55yrs old man presented vtha) hypoglycemic episodes ? sec to drug induced b)hypoalbunemia ?sec to renal failure (spot protein/creat ratio 3.19) 24hrs urine protein not available?
as diabetic nephropathy is leading cause for renal failure. c)anemia(hb 9.7)
2) in this pt could be due to? drug induced.
Glimepiride is metabolized by the liver to two major metabolites each of which has hypoglycemic activity. In renal disease these metabolites summed. Although the half-life is 5-7 h, the drug can cause severe hypoglycemia that lasts more than 24hrs. along vth insulin clearence is reduced.
Evaluation of hypoglycemia:
3) pathophysiology of hypoglycemia: activayes pro inflammatory,pro coagulant,pro thrombotic respones incplatelet agg,reduce fibronoytic balance,inc intravascular coagulation.
4)causes to dyspnea could be cardiac: heart failure,pulmonary: pneumonia,copd, anemia and many other causes.Acc to data available could be due to ?anemia.
QUESTION NO 3 A)
1) In this patient as eular criteria score is 7 for further evauation anticcp antibodies can be send in diff RA from other polyarticular devices as it is ass vth other chronic inflammatory conditions..
it is more specific than RAfactor in diagnosing and may predict erosive disease more effectively.
Radiography of joints : intial finding in RA is PERIARTICULAR OSTEOPENIA. others include symmetric joint space loss,subchondral erosions(mostly seen in wrists and hands).In advanced stages
signs of sev destruction vth joint sublaxation and collapse..
2) pathogenesis of RA:

3)Treatment regimens:
the intial treatment was conservative and NSAIDS for pain relief for several yrs and only progressing to DMARDS when the dis was not Controlled.
DMARDs possess a slow onset of action, and response to treatment is usually expect- ed between 4-6months.
Sulfasalazine and methotrexate are gener- ally regarded as first line therapies due to their improved efficacy profile (approxi- mately 40 per cent response rates) and high continuation rates compared to the other DMARDs.
Steroids: Systemic corticosteroids have long been used in the management of RA and were the first drugs to result in reversibility of the disease.
Oral prednisolone can be used to provide temporary relief until a DMARD becomes effective, or in patients with aggressive disease who cannot be ade- quately controlled with a combination of DMARDs (“step-up” or “step-down” approach).
TNF blockade : at the present time, agents for TNF blockade are only used in patients that are resistant to, or fail conventional disease- modifying treatment
QUESTION NO 3B
1) As pt is having febrile reaction during 1st transfusion ( feverspikes were present ) repeat lft was not available to rule out whether there is any acute hemolytic reaction.
later during 2nd transfusion post op pt had another febrile reaction vth elevated bilirubin and sr ldh levels. this could be delayed hemolytic reaction ( indirect coombs test- positive) vth mixed hyperbilirubinemia
pt could be having ischemic hepatitis ( as there is intraop hypotension episode and post op too).
2) supportive managment with iv fluids . and pt coagulation profile is derranged inj vit k can be given. and pain managment.
QUESTION NO 4
1.60 year old female with T2DM c/o pricking type of chest pain since 4 days and uncontrolled sugars secondary to ? right upper lobe pneumonic consolidation with sepsis
2. What are the factors contributing to her uncontrolled blood sugars?
Ans:
3. What are the chest xray findings?
Ans:
Plain radiograph of chest , frontal view
Trachea shifted towards right
Hyperdense area noted in the right upper lobe
(consolidation)
Peripheral pulmonary vasculature is normal
Heart is central in position
Cardiac size normal
The domes of diaphragm are normal in position and smooth outline
Visualized bones and soft tissue appear normal
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
Ans: Inflammation (acute phase reactant)
Malnutrition
Albuminuria (protein losing nephropathy)
5. Comment on the treatment given along with each of their efficacies with supportive evidence.
- Piptaz & clarithromycin : for his right upper lobe pneumonic consolidation and sepsis
- Egg white & protien powder : for hypoalbuminemia
- Lactulose : for constipation
- Actrapid / Mixtard : for hyperglycemia
- Tramadol : for pain management
- Pantop : to prevent gastritis
- Zofer : to prevent vomitings
QUESTION NO 5
1) according to history anatomical localisation was liver involvement as pt was diagnosed to have
HEP B since 2yrs. and he is k/c/o alcoholic due to which pt has chronic liver failure leading
to ascites,portal htn, jaundice, hypoalbunemia, gi bleeds,
pt has renal failure could be due to hepb virus infection.
it could cause either PAN/MPGN/HEPATORENAL SYNDROME
In this pt could be? hepatorenal syndrome( cue not vaialable? to rule out glomerular injury causing albuminuria,hematuria)
2) evaluation of hep b:



3) pathogenesis :
4) Some people who are receiving dialysis treatment have virus infection such as hepatitis B, hepatitis C and/or HIV that is present in their blood. These infections can be transmitted to other patients if blood is contaminated by the blood of another with a viral infection. Haemodialysis is performed by passing blood from a patient through a dialysis machine, and multiple patients receive dialysis within a dialysis unit. Therefore, there is a risk that these viruses may be transmitted around the dialysis session.
5) There is evidence to support the use of octreotide in variceal and non-variceal upper GI bleeding (UGB). As a somatostatin analogue, octreotide binds with endothelial cell somatostatin receptors, inducing strong, rapid and prolonged vaso-constriction [1]. Octreotide reduces portal and variceal pressures as well as splanchnic and portal-systemic collateral blood flows [2]. It also prevents postprandial splanchnic hyperemia in patients with portal hypertension [3] and lowers gastric mucosal blood flow in normal and portal hypertensive stomachs [4]. Octreotide inhibits both acid and pepsin secretion. As a result, it prevents the dissolution of freshly formed clots at the site of bleeding [5]. In several studies on HBV-infected patients, the vast majority with LAM-resistant virus, TDF 300 mg once daily resulted in a reduction of 4 to 6 log10 copies/mL in serum HBV DNA level from baseline over 48 weeks and in reduction of 5 log10 copies/mL compared with placebo; also HBV DNA was undetectable by PCR assay in 30% to 100% of patients after more than 24 weeks treatment
QUESTION NO 6
1) As pt having h/o unable to do his weaving work properly sin 1yr ,forgetfullness of things, unintentionally picking of objects,urinary incontinence, suggests of temporal and parietal lobe involvement.
pt having slurring of speech,difficulty in swallowing could be due to cranial nerve involvement
as dementia progress(sev type)
2) evaluation : https://www.aafp.org/afp/2018/0315/p398.html#afp20180315p398-t3
https://www.aafp.org/afp/2018/0315/p398.html#afp20180315p398-t3
3)Vascular dementia symptoms vary, depending on the part of your brain where blood flow is impaired. Symptoms often overlap with those of other types of dementia, especially Alzheimer's disease dementia.
Vascular dementia signs and symptoms include:
- Confusion
- Trouble paying attention and concentrating
- Reduced ability to organize thoughts or actions
- Decline in ability to analyze a situation, develop an effective plan and communicate that plan to others
- Difficulty deciding what to do next
- Problems with memory
- Restlessness and agitation
- Unsteady gait
- Sudden or frequent urge to urinate or inability to control passing urine
- Depression or apathy
- Sometimes a characteristic pattern of vascular dementia symptoms follows a series of strokes or ministrokes. Changes in your thought processes occur in noticeable steps downward from your previous level of function, unlike the gradual, steady decline that typically occurs in Alzheimer's disease dementia.
- https://www.mayoclinic.org/diseases-conditions/vascular-dementia/symptoms-causes/syc-20378793
-
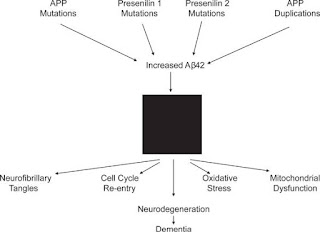
4) In this pt cause could be ALZHEIMERS DISEASE pathogenesis is
The first defined histopathologic features of AD were extracellular amyloid plaques and intracellular neurofibrillary tangles. More recently recognized histopathologic features include synaptic degeneration, hippocampal neuronal loss, and aneuploidy.
5) treatment modalities:
Donepezil is used to treat confusion (dementia) related to Alzheimer's disease. It does not cure Alzheimer's disease, but it may improve memory, awareness, and the ability to function. This medication is an enzyme blocker that works by restoring the balance of natural substances (neurotransmitters) in the brain.
On average, most studies with AChEIs reported by the pharmaceutical industry showed a cognitive enhancement of 2–3 points (vs placebo) in the ADAS-Cog score in clinical trials of 12–30 weeks’ duration, with improvement in 12%–58% of patients, 5%–73% of drop-outs, and side-effects in 2%–58% of cases . As compared with other AChEIs, donepezil exhibits the best pharmacological profile in terms of cognitive improvement (2.8–4.6 vs 0.7–1 points of difference with placebo in the ADAS-Cog scale), responders rate (40%–58%), drop-out cases (5%–13%), and side-effects (6%–13%
QUESTION NO 7
1) 22yrs old male presented with c/o intermittent tonic type of seziure since 2months , along vth h/o fever low grade on and off, weight loss,dec appetite.
On/e: pt having lft supraclavicular lymphadenopathy, vth lft axillary lymphadenopathy vth dec breathsounds on lt side
Mri shows- ring enhancing lesions in lt cerebellum region
Could be the possibility of ? TUBERCULOMA
Primaryfocus from lung has to be confirmed vth sputum studies report..
Hiv status of the pt??
It results from the hematogenous dissemination of Mycobacterium tuberculosis from disease elsewhere in the body and the formation of small subpial and subependymal foci in the brain and spinal cord. In some individuals, these foci rupture and release bacteria into the subarachnoid space, causing meningitis.
Magnetic resonance spectroscopy of normal brain shows predominant peaks of N-acetylaspartate (NAA), choline, creatinine and myo-inositol with the highest peak being NAA. NAA is a healthy neuronal marker, choline represents energy store and choline is a marker of cellular turnover
Magnetic resonance spectroscopy is of great value in the diagnosis of tuberculoma in cases of ring-enhancing lesions on CT scan or MRI imaging. It demonstrates a very high lipid peak, reduction in NAA and creatinine and a choline/creatinine ratio of >1 Lipid peak in MRS in the context of a ring-enhancing lesion is very much specific for tuberculoma and has not been seen in any cases of NCC, the other common differential diagnosis of a ring-enhancing lesion. NCC demonstrates a high lactate and proteins like alanine, succinate, glutamate, glycine levels with some reduction of NAA and creatinine A high choline peak is seen in MRS in case of tumors, primary or secondary, because of very high cellular turnover. MRS can also differentiate tuberculoma or tuberculous brain abscess from pyogenic brain abscess by the presence of elevated levels of amino acid peaks in pyogenic brain abscess.
2) DD for ring enhancing lesions:
3)A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome (IRIS).
BHIVA has issued guidelines[11] for starting the TB treatment with HAART. If CD4+ count is less than 100 cells/μl, both anti-tuberculosis drugs and HAART can be started together. If CD4+ cells are in the range of 100-200; HAART is started 2 months after starting TB treatment. If the CD4+ cells are above 200, HAART is started 6 months after completing TB treatment. QUESTION NO8)
Dec 1st - read about mechanisms of actions of anti epileptic drugs
Dec 2nd- acute dysentery etiologies
Dec 3rd- Read about dengue pathophysiology
Dec4th- followed rounds
Dec 5th- Duty day
Dec 6th- read about hypertension emergency and management
Dec 7th- read about the approach in treatment of GTCS type,focal type seizures and status epilepticus .
Dec 8th- read about the approach to hypoalbunemia and its causes. Read about the iron def anemia.
Dec 9th - read about peripheral vascular disease and examination
Dec 10th - read about Heart failure pathophysiology
Dec11th - read about Acute pancreatitis
Dec 12th - duty day
Dec13th- read about the pathophysiology of heart failure and types of cardiorenal syndromes and its mechanisms. And wet Beto beri
Dec 14th - read about Parkinson’s disease and atypical parksonism
Dec 15th- read about type of dementia and how to differentiate from each type.
Dec16th - attended rounds and 2-4 discussion disscused difference btwndry and wet gangrene, tretmentof heart failure who is in cardiogenic shock.




















Comments
Post a Comment