BI MONTHLY ASSESSMENT MAY 2021
Pulmonology
A) Link to patient details:
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology and Event timeline-
20 Years ago - SOB Grade1 for a week , occurred every year for the same duration
18 Years ago- Polyuria and was diagnosed with DM
12 Years ago - SOB Grade 1 for a month
1 Month ago - Weakness was given iv fluids
30 Days ago - SOB ( latest episode) gradually progressive
20 Days ago - HRCT showed Bronchiectasis
15 Days ago - Pedal edema and facial puffiness
2 Days ago - SOB Grade 4 , drowsiness and decreased urine output.
Anatomical location of the problem is BRONCHIOLES,RIGHT heart failure(Cor pulmonale)
Primary etiology is rice dust exposure as patient is a farmer working in paddy fields,home chulla usage
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
TREATMENT:
Head end elevation
Decreases the risk of aspiration as the patient is drowsy
O2 inhalation to maintain SPO2 above 92%
Oxygen inhalation as her spo2 is low
Intermittent BiPAP for 2hrs
the utility of NIV in acute hypercapnic respiratory failure in copd is well-established. since the mid-1990’s, studies have demonstrated superior outcomes in patients with hypercapnic respiratory failure during copd exacerbation when treated with niv compared to management without niv (1,2). it is now a standard component of the management of these patients and is included in the most recent international guidelines (3,4). established criteria for patient selection include persistent acidosis (ph <7.35), hypercapnia (pco2 >6.5 kpa) or tachypnoea (respiratory rate >22 breaths per minute) despite optimal bronchodilator and controlled oxygen therapy (3). despite these standardised criteria and increasing experience with niv therapy outside of the critical care setting, the rate of failure of niv therapy is still reported to be as high as 20–30%
When compared with invasive mechanical ventilation in randomised clinical trials, observational cohorts or meta-analyses, NIV has been shown to have better outcomes (reduced inpatient mortality and length of stay) (1,8,9). This can be explained by a higher complication rate in the group treated with invasive mechanical ventilation. The need for NIV in acute exacerbations of COPD itself continues to be a poor prognostic factor. In a cohort of 757 patients admitted to hospital with an acute exacerbation of COPD, treatment with NIV was an independent marker of 1-year mortality
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803033/
TAB. AZITHROMYCIN 500mg OD
Inj. AUGUMENTIN 1.2gm IV BO
Augmentin - Amoxicillin + Clavulanic acid.
MECANISM OF ACTION:
Amoxicillin is in the class of beta-lactam antimicrobials. Beta-lactams act by binding to penicillin-binding proteins that inhibit a process called transpeptidation (cross-linking process in cell wall synthesis), leading to activation of autolytic enzymes in the bacterial cell wall
Clavulanic acid contains a beta-lactam ring and binds strongly to beta-lactamase at or near its active site, thereby hindering enzymatic activity. This protects other beta-lactam antibiotics from beta-lactamase catalysis, thereby enhancing their antibacterial effects
P:enrolled children aged 1-19 years with radiographically proven bronchiectasis unrelated to cystic fibrosis.
I,C At the start of an exacerbation, children were randomly assigned to oral suspensions of either amoxicillin-clavulanate (22·5 mg/kg, twice daily) and placebo or azithromycin (5 mg/kg per day) and placebo for 21 days
O screened 604 children and enrolled 236. 179 children had an exacerbation and were assigned to treatment: 97 to amoxicillin-clavulanate, 82 to azithromycin). By day 21, 61 (84%) of 73 exacerbations had resolved in the azithromycin group versus 73 (84%) of 87 in the amoxicillin-clavulanate group. The risk difference showed non-inferiority (-0·3%, 95% CI -11·8 to 11·1). Exacerbations were significantly shorter in the amoxicillin-clavulanate group than in the azithromycin group (median 10 days [IQR 6-15] vs 14 days [8-16]; p=0·014). Adverse events were attributed to the trial medication in 17 (21%) of 82 children in the azithromycin group versus 23 (24%) of 97 in the amoxicillin-clavulanate group (relative risk 0·9, 95% CI 0·5 to 1·5).
Interpretation: By 21 days of treatment, azithromycin is non-inferior to amoxicillin-clavulanate for resolving exacerbations in children with non-severe bronchiectasis. In some patients, such as those with penicillin hypersensitivity or those likely to have poor adherence, azithromycin provides another option for treating exacerbations, but must be balanced with risk of treatment failure (within a 20% margin), longer exacerbation duration, and the risk of inducing macrolide resistance.
https://pubmed.ncbi.nlm.nih.gov/30241722/
INJ. LASIX IV BO if SBP greater than 110 mmHg
To reduce the peripheral volume overload due to right heart failure
INJ. HYDROCORTISONE 100 mg IV
The administration of corticosteroids in the treatment of AECOPD was assessed. In comparison to placebo, systemic corticosteroids improve airflow, decrease the rate of treatment failure and risk of relapse, and may improve symptoms and decrease the length of hospital stay. Therefore, corticosteroids are recommended by all major guidelines in the treatment of AECOPD. Existing literature suggests that low-dose oral corticosteroids are as efficacious as high-dose, intravenous corticosteroid regimens, while minimizing adverse effects. Recent data suggest that shorter durations of corticosteroid therapy are as efficacious as the traditional treatment durations currently recommended by guidelines.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4014384/
NEB. with IPRAVENT, BUDECORT 6 hrly
TAB PULMOCLEAR 100 mg PO OD
Acebrophylline+acetylcystine
Acetylcystine is mucolytic,makes the secretions thin
Acebrophylline is a bronchidilator which helps in clearance of those thinned out secretions
chest physiotherapy
It is done to make the patient cough out the secretions and sputum
GRBS 6 hrly
INJ. HAI SC ( 8 am- 2pm- 8pm)
Rapid acting insulin for sugar control
Temp, BP, PR, SPO2 monitoring
I/O charting
INJ. THIAMINE 1 amp in 100 ml of NS
As patient is alcoholic thiamine deficiency may also contribute to right heart failure,so thiamine supplementation was given
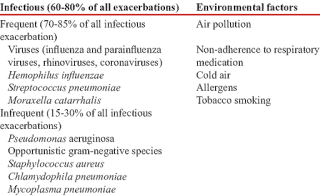
3) What could be the causes for her current acute exacerbation?
The patient may have infectious or non infectious cause of exacerbation.And may be this time her right heart failure got even worsesned which made her present to hospital
4. Could the ATT have affected her symptoms? If so how?
Did not find any case report with ATT causing copd exacerbaration
5.What could be the causes for her electrolyte imbalance?
Patients with COPD tend to retain sodium. In addition, serum potassium should be monitored carefully, because diuretics, beta-adrenergic agonists, and theophylline act to lower potassium levels.
Beta-adrenergic agonists also increase renal excretion of serum calcium and magnesium, which may be important in the presence of hypokalemia.
Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD.
https://www.medscape.com/answers/297664-7379/which-electrolyte-levels-should-be-monitored-in-patients-with-chronic-obstructive-pulmonary-disease-copd#:~:text=Patients%20with%20COPD%20tend%20to,act%20to%20lower%20potassium%20levels.
Neurology (10 Marks)
A) Link to patient details:
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
Chronic alcoholic since 12 yrs
Diabetes since 2 yrs (irregular medications)
2-3 episodes of seizures in last 1 year
Irrelevant talking , forgetfulness and decreased food intake since 9 days.
Anatomical localization:
Brain : Wernicke's Encephalopathy
Kidney : AKI (pre-renal sec to ?dehydration)
Primary etiology:
Alcohol
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Thiamine: correction of thiamine deficiency
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7163251/
KCL & Potchlor: correction of hypokalemia
https://emedicine.medscape.com/article/242008-treatment#d9
Lorazepam: to treat alcohol withdrawl
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606320/
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
This time he may have developed wernicke's encephalopathy.
Or it may be due to uremic encephalopathy.
Or it may because of kindling in alcohol withdrawl where repeated withdrawls will lead to more severe symptoms.
4) What is the reason for giving thiamine in this patient?
5) What is the probable reason for kidney injury in this patient?
Alcohol - osmotic diuresis - dehydration - pre renal AKI
6). What is the probable cause for the normocytic anemia?
Alcohol abuse and dependence can cause normocytic normochromic anemia through:
Decreased red blood cell production in the bone marrow - Normocytic normochromic anemia
Loss of blood through ulcers or inflammation - Iron deficiency anemia which in normocytic normochromic in early stages
Destruction of red blood cells from heart valve issues, inflammation, immune system damage, or a cancerous tumor - Normocytic normochromic anemia
https://www.alcohol.org/effects/anemia/
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Chronic alcoholism may lead to foot ulcer formation and delayed healing due to alcoholic neuropathy & malnutrition.
B) Link to patient details:
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
Chronic alcoholic & smoker since 30 yrs
!
Giddiness & vomiting 7 days back (relieved with rest)
!
Giddinesss , vomiting , b/l hearing loss , aural fullness , tinnitus , ataxia since 4 days
!
Deviation of mouth & slurring of speech since 1 day
Anatomical localization:
Brain - cerebellar involvement
Primary etiology:
Acute infarct in right inferior cerebellar hemisphere
Risk factors in this patient : Alcohol / Smoking / Denovo HTN
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
VERTIN:
This is betahistine, which is an anti-vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
ZOFER:
This is ondanseteron- It is an anti-emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
ECOSPIRIN
This is aspirin. It is an NSAID (anti-platelet)
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis.
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
CLOPIDOGREL:
It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting.
ATORVASTATIN:
This is a statin group of drug
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
THIAMINE:
It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
3) Did the patients history of denovo HTN contribute to his current condition?
Yes
Hypertension is a risk factor for CVA
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Epidemological studies indicate mild to moderate amount of alcohol consumption is protective in ischemic stroke.
Heavy alcohol consumption was associated with increased risk of intracerebral hemorrhage and hemorragic stroke.
https://www.researchgate.net/publication/316523838_Alcohol_use_and_risk_of_intracerebral_hemorrhage
Recent heavy alcohol consumption can increase risk for all major types of stroke.
The pathophysiologic mechanisms by which alcohol triggers the onset of spontaneous intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage and ischemic brain infarction remain largely unresolved.
https://documentcloud.adobe.com/link/review?uri=urn:aaid:scds:US:32bf4e92-ca76-4e0d-973d-f21152c018e0
C) Link to patient details:
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
B/l pedal edema since 8 months
Dragging type of pain in left UL ass with tingling & numbness
Chest pain , palpitations & SOB grade-III since 5 days
Anatomical localization:
Based on the clinical history & limited investigations (ECG not available)
Heart - ? NSTEMI
Primary etiology:
? CAD
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Based on the available data it is difficult to comment on the reason for recurrent hypokalemia.Further evaluation is needed
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
D) Link to patient details:
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Mechanism of seizure following brain stroke
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Previous episode of seizure was a focal seizure
Now the seizure was of focal with secondary generalisation ,GTCS due to which the patient had loss of consciousness
E) Link to patient details:
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
In this patient ataxia may be secondary to chronic alcoholism.
ALCOHOL INDUCED CEREBELLAR DEGENERATION
Alcohol-induced cerebellar degeneration is the commonest type of acquired toxic ataxia. The onset of the cerebellar symptoms usually occurs at middle age, with a significant history of chronic alcohol abuse. Permanent cerebellar deficits are observed among alcoholics, and they persist even with alcoholic abstinence. The cerebellum is the structure that controls the stability of the gaze, chronic cerebellar diseases and acute alcohol intoxication affect cerebellar function. Ataxia and nystagmus are neurological manifestations present in this disease. To verify vestibulocochlear disorders observed in a case of alcohol-induced cerebellar ataxia.
https://www.sciencedirect.com/science/article/abs/pii/S0987705319303351#:~:text=Alcohol%2Dinduced%20cerebellar%20degeneration%20is,persist%20even%20with%20alcoholic%20abstinence.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Analyses demonstrated an association of rare and moderate alcohol consumption with decreased risk of both lobar and nonlobar ICH. Heavy alcohol consumption demonstrated a strong association with increased nonlobar ICH risk.
Study demonstrated potential protective effects of rare and moderate alcohol consumption on ICH risk. Heavy alcohol consumption was associated with increased ICH risk. Race/ethnicity was a significant factor in alcohol-associated ICH risk; heavy alcohol consumption in black and Hispanic participants poses significant nonlobar ICH risk.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440244/
F) Link to patient details:
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
No
2.What are warning signs of CVA?
3.What is the drug rationale in CVA?
1.Injection Mannitol 100ml/IV/TD
prospectively studied 922 consecutive patients admitted with acute ischemic stroke. Patients who showed space-occupying brain edema with tissue shifts compressing the midline structures received mannitol. The outcome was assessed with dependency rates at discharge (modified Rankin Scale grade 2-5) and in-hospital mortality. Rates of dependency were higher in patients treated with mannitol (n = 86) than in those who were not (97.7 and 58.5%, respectively; p < 0.001). Independent predictors of dependency were age, history of ischemic stroke and National Institutes of Health Stroke Scale (NIHSS) score at admission. Rates of mortality were higher in patients treated with mannitol than in those who were not (46.5 and 5.6%, respectively; p < 0.001). Independent predictors of in-hospital mortality were diastolic blood pressure [relative risk (RR) 1.05, 95% confidence interval (CI) 1.02-1.08, p < 0.001], NIHSS score at admission (RR 1.19, 95% CI 1.14-1.23, p < 0.001) and treatment with mannitol (RR 3.45, 95% CI 1.55-7.69, p < 0.005).
Conclusions: Administration of mannitol to patients with ischemic stroke-related cerebral edema does not appear to affect the functional outcome and might increase mortality, independently of stroke severity.
https://pubmed.ncbi.nlm.nih.gov/29845546/
2.TAB Ecospirin 75 mg po/OD
ECOSPIRIN
This is aspirin. It is an NSAID (anti-platelet)
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis.
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
3.TAB ATORVAS 40mg po/HS
This is a statin group of drug
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
4. Does alcohol has any role in his attack?
Many risk factors are linked to the likelihood of having a stroke. Some of these include:
- High blood pressure is one of the top risk factors for stroke, and it contributes to more than half of all strokes.
- Diabetes doubles the risk of having a stroke.
- People who are overweight are at a higher risk of having a stroke.
- Something called atrial fibrillation which is a situation where you have an irregular heartbeat can increase the chances of having a stroke by as much as five times.
- Liver damage can cause your liver to stop making certain substances that help in the clotting of blood, so this can increase the risk of stroke.
What’s important to realize with all of the above risk factors is the fact that they can all also be linked to alcohol, which is why there is a link between alcohol and stroke. Can alcohol cause a stroke? Yes, in many ways alcohol can increase the chances of having a stroke.
https://www.therecoveryvillage.com/alcohol-abuse/faq/alcohol-and-stroke/
5.Does his lipid profile has any role for his attack??
His lipid profile is within normal limits
G) Link to patient details:
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
__*Questions*_
1)What is myelopathy hand ?
The “myelopathy hand” in cervical spondylosis includes findings of localised wasting and weakness of the extrinsic and intrinsic muscles of the handThere is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers.
These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement in various cervical spinal disorders when there is involvement of the spinal cor
Intrinsic muscle wasting & positive finger escape present.
2)What is finger escape ?
The finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign". Upper motor neuron disorders of the cerebral cortex such as mild hemiplegic stroke or hemiplegic migraine where the same clinical finding has been called the "digiti quinti sign".
3)What is Hoffman’s reflex?
Hoffmann's reflex (Hoffmann's sign, sometimes simply " Hoffmann's ", also finger flexor reflex) is a neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from the corticospinal tract. It is named after neurologist Johann Hoffmann.
H) Link to patient details:
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
Possible questions:
1) What can be the cause of her condition ?
Acute cortical vein thrombosis with hemorrhagic venous infarction involving right posterior temporal lobe.
2) What are the risk factors for cortical vein thrombosis?
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Initially patient was completly sedated with midazolam infusion and achieved a seizure free period f/b 1-2 episodes of recurrence after tapering the dose of midazolam
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulation
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
3) Cardiology (10 Marks)
A) Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html.
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
2.Why haven't we done pericardiocenetis in this pateint?
This patient had no cardiac tamponade which is an absolute indication for pericardiocentesis.
So we treated him conservatively considering the risks associated with the procedure.
If he had developed cardiac tamponade at any point of time we would have immediately done a pericardiocentesis.
3.What are the risk factors for development of heart failure in the patient?
NON MODIFICABLE:
age
gender
MODIFIABLE:
hypertension
smoking
type 2 diabetes .
kidney disease.
4.What could be the cause for hypotension in this patient?
B) Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html.
Questions:
1.What are the possible causes for heart failure in this patient?
obesity
alcohol
diabetes
hypertension
2.what is the reason for anaemia in this case?
It could be anemia of chronic disease secondary to chronic kidney disease and chronic heart failure
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
The pt. had recurrent blebs and ulcer on lower limbs (foot). This is due to Type 2 diabetes mellitus.
Diabetic foot ulcers generally arise as a result of poor circulation in the foot region. While high blood sugar levels and nerve damage or even wounds in the feet may result in foot ulcers in many cases.
In cases of poor circulation of blood, the foot ulcers take quite a bit of time to heal as the blood efficiency in the foot region is at a low level. Furthermore, many develop a bit of reduced sensation on the feet as a result of nerve damage or more.
There are many risk factors that may lead to foot ulcers at the end.
Poor quality or fitting of the footwear.
Unhygienic appearance of foot.
Improper care of the nails of the toe.
Heavy intake of alcohols and tobacco.
Obesity and Weight-related
Complication arising from Diabetes like eye problems, kidney problems and more.
Although aging or old age can also be counted among them.
4. What sequence of stages of diabetes has been noted in this patient?
Alcohol------obesity------impaired glucose tolerance------diabetes mellitus------microvascular complications like triopathy and diabetic foot ulcer-------macrovascular complications like coronary artery disease , coronary vascular disease and peripheral vascular disease.
C) Link to patient details:
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?:
Symptomatology and events
Chronic alcoholic
!
NSAID abuse since 3 yrs
!
Facial Puffiness on & off since 2-3 yrs
!
HTN since 1 year
!
SOB grade : II - IV & decreased urine output since 2 days
!
Anuria since 1 day
!
Denovo DM
Anatomical localization:
Kidney : CKD (?Analgesic Nephropathy)
Heart : HFrEF (?CAD)
Primary etiology:
NSAID abuse
CKD
HTN
T2DM
CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1. TAB.DYTOR
Mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB.ACITROM
Mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. CARDIVAS
Mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
Mechanism: Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue.
5.TAB. DIGOXIN
Meechanism: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Patient has cardiorenal syndorme type 4
4) What are the risk factors for atherosclerosis in this patient?
Hypertension and obesity,old age,diabetes mellitus, Alcohol
5) Why was the patient asked to get those APTT, INR tests for review?
Patient was kept on T.ACITROM (ACENOCOUMARAL) which is an anti coagulant and was discharged.
So to moniter the response to treatment & maintain it within a therapeutic range, to provide the benefits of anticoagulation, while avoiding the risks of haemorrhage PT , INR & APTT are monitored frequently.
D) Link to patient details:
https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
T2DM since 12 yrs
!
On & off chest pain since 1 year
!
TB 7 months back - used ATT for 6 months
!
HTN since 6 months
!
Profuse sweating & SOB grade : III - IV since 30 min
Anatomical localization:
Heart : CAD : NSTEMI
Primary etiology:
T2DM & HTN - CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVC.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Over diagnosis is which occurs when a true abnormality is discovered, but detection of that abnormality and its treatment does not benefit the patient.
Over diagnosis will lead to over treatment , psychological effects & economic burden.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586591/#
To prevent these adverse events more research is important in this over diagnosis & over treatment
E) Link to patient details:
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
T2DM & HTN since 8 yrs
!
Chest pain since 3 days
!
Giddiness & profuse sweating since 1 day
Anatomical localization:
Heart : Inferior wall MI
Primary etiology:
Acute inferior wall MI
T2DM , HTN leading to CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Aspirin, clopidogrel
Atorvas
CLINICAL INDICATIONS OF PTCA:
Acute ST - elevation myocardial infarction ( STEMI )
Non ST - elevation acute coronary syndrome ( NSTE-ACS )
Unstable angina
Stable angina
Anginal equivalent (eg; dyspnoea, arrhythmia, or dizziness or syncope )
High risk stress test findings.
https://www.ncbi.nlm.nih.gov/books/NBK535417
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Secondary PTCA was unnecessary in the patient as he already crossed the window period of 12 hours and was doing fine without PTCA.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768296
F) Link to patient details:
https://kattekolasathwik.blogspot.com/2021/05/a-case-of-cardiogenic-shock.h
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
History is not clear
2. What is the rationale of using torsemide in this patient?
Torsemide : loop diuretic
This patient is in fluid overload & heart failure where diuretics are the main stay of treatment (reducing preload)
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
No its not prophylactic
H/o whitish discharge & TLC was 18000 which clearly indicates infection for which ceftriaxone was given.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS:
5years ago- developed pain abdomen and vomiting
1 week ago- developed pain abdomen
4days ago- developed fever , constipation and burning micturition.
Anatomical localization in the patient is Pancreas.
Primary etiology of the condition is chronic alcohol intake.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS:
drugs used are meropenem , metrogyl , amikacin , octreotide and thiamine.
Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
INJ.TRAMADOL
*It is opiod analgesic used for pain relief.
B) Link to patient details:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
ANS:
The patient has mild b/l pleural effusion which may be causing his dyspnea.
Two main causes of pleural effusion are:
• Transdiaphragmatic lymphatic blockage leading to increased permiability.
• Pancreaticopleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis.
These changes are mediated by inflammatory cytokines.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4087768/
A sudden onset, severe upper abdominal pain in a patient looking very unwell is a very highly suggestive of pancreatitis. Occasionally, the patient may also have slight shortness of breath or painful breathing if the inflammation encroaches onto the lower part of the lung.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
ANS:
Pancreatitis is nothing but the inflammation of the pancreas. Acute pancreatitis is caused when such an inflammation of the pancreas comes all of a sudden and brings the acute amount of pain.
Pancreas that is mainly responsible for the production of the hormone, insulin. However, when the organ gets inflammation due to various reasons, the cells in the pancreas that are responsible for the production of the hormone are damaged. Thus, diabetes is caused. Thus, as a result of pancreatitis, a patient will require administering insulin through various external sources. The most common form of diabetes that is mainly known to be caused as a result of the pancreatitis is known as secondary diabetes.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
ANS:
The liver is one of the largest and most complex organs in the body. It is the chief organ responsible for metabolizing alcohol and is especially vulnerable to alcohol related injuries.
As alcohol is broken down inside the liver, it releases a number of potentially dangerous byproducts that may damage the liver more than the alcohol itself
Each of these toxins plays a role in the damage of the liver and the subsequent release of enzymes from the cells
Heavy drinking for as little as just a few days can lead to fatty liver, the earliest stages of alcoholic liver disease
Specific markers for Alcoholic Liver Disease:
•AST level is more than twice that of ALT
• Elevated levels of Gamma Glutamyl Transferase (GGT)
https://pubs.niaaa.nih.gov/publications/aa64/aa64.htm
4) What is the line of treatment in this patient?
ANS;
For the master chart to the "pancreatitis thesis project" please get in touch with Dr Shashikala PGY1 and Dr Divya PGY2 and share their insights into the above project problem they are working on.
C) Link to patient details:
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
Possible Questions :-
1) what is the most probable diagnosis in this patient?
ANS:
Ruptured liver abscess and organised collection secondary to hollw viscus perforation
2) What was the cause of her death?
SEPSIS with MODS
But again etiology can be confirmed only by exploratory laporotomy.
3) Does her NSAID abuse have something to do with her condition? How?
If at all it is a hollow viscus perforation it can be secondary to her NSAID abuse.
https://www.medscape.com/viewarticle/437220#:
NSAID abuse may lead to grade-3 RPD changes in kidney
CKD (?Analgesic Nephropathy)
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
1. What could be the reason for his SOB ?
ANS: Metabolic acidosis, pulmonary edema,anemia causing heart failure
2. Why does he have intermittent episodes of drowsiness ?
ANS:
Hyponatremia and decrease in the renal clearance of waste nitrogenous products accompanies with their continuous generation leads to diverse uremic retention products such as urea, creatinine, guanidine and homocysteine. Many of these toxins affect functioning of cells and organs, resulting in endothelial vascular injury, neurotoxicity and cognitive dysfunction.
Taken from the following article -
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6312775/
3. Why did he complaint of fleshy mass like passage in his urine?
ANS:
The fleshy mass like passage in his urine might be
the fleshy tissues of prostate post TURP or excessive pus cells in the urine (according to the reports) and the frothy appearance may be due to the presence of proteins. The urine is pale yellow in colour.
4. What are the complications of TURP that he may have had?
ANS:
A complication of TURP that the patient may have had is 'TURP syndrome'.
It is rare but is life threatening.
Cause- It may occur as a consequence of absorption of fluids used to irrigate the bladder during the operation.
Signs and symptoms are due to fluid overload and electrolyte disturbances and hyponatremia.
B) Link to patient details:
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
ANS:
One possible Provisional diagnosis of this patient is ADHD (Attention deficit/Hyperactive disorder).
Symptoms may start before the age of 12 and include inattention and hyper active impulsive behavior.
Inattention -
They have trouble to stay focused in tasks or play.
They appear not to listen even when spoken directly.
They are easily distracted.
They avoid or dislike tasks that require mental effort.
Hyper active impulsive -
Have difficulty sitting in one place and are always on the run.
Fidget with their hands or legs.
Talk too much
Have difficulty waiting for their turn.
Academic difficulties are frequent as are problems with relationships.
2. Why doesn't the child have the excessive urge of urination at night time ?
ANS:
It maybe Psychosomatic. The child has the urge to urinate in the morning due to stress or mental conflict. During sleep, the kid is free of stress and may not have the urge to urinate excessively.
3. How would you want to manage the patient to relieve him of his symptoms?
ANS:
The only management is reassurance to the kid and his relaxation by reducing stress. The problem will resolve overtime (most commonly by the time he reaches 10yrs).
There are a variety of psychotherapeutic approaches employed by psychologists and psychiatrists; the one used depends on the patient and the patient's symptoms. The approaches include psychotherapy, cognitive-behavior therapy, support groups, parent training, meditation, and social skills training.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
ANS:
Clinical history- weight loss, recurrent chest infections, trauma, malignancy or ingestion of caustic substances, pyrexia of unknown origin
Physical findings- Uncontrolled coughing after swallowing, often worse with carbonated drinks (ONO sign).
Barium swallow done for dysphagia
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANS:
As this patients latest CD4 count is 91, i think we need to stop ART and start ATT f/b ART initiation 6-8 wks later to prevent IRIS
7) Infectious disease and Hepatology:
Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?What could be the cause in this patient ?
ANS:
Alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver.
Though Alcoholism is a predisposing factor, it has no role in the aetiology and the liver function tests also did not show much alteration.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
ANS:
Amoebic liver abscess is more common than pyogenic liver abscess. Commonly occurs in young alcoholic males.
Alcohol is only the predisposing factor of liver abscess but not the true etiological agent. Chronic alcoholism leads to Fatty liver and liver cirrhosis (Alcohol liver disease) which eventually results in liver abscess if liver is infected with entamoeba histolytica or other pathogenic organisms.
3. Is liver abscess more common in right lobe ?
ANS:
When the infection spreads to the liver through the portal veins it arises more commonly in the right lobe, probably due to an unequal distribution of superior and inferior mesenteric vein contents within the portal venous distribution. A plain abdominal radiograph is not sensitive for evaluating liver abscesses.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
ANS:
1) If the abscess is large ( 5cm or more) because it has more chances to rupture.
2) If the abscess is present in left lobe as it may increase the chance of peritoneal leak and pericardial leak.
3) If the abscess is not responding to the drugs for 7 or more days .
B) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
QUESTIONS:
1) Cause of liver abcess in this patient ?
ANS:
Cause of liver abcess may be due to contamination of food / fluid history of which is not mentioned.
malnutrition and poor personal hygiene are also the risk factors of liver abcess.
The cause for abscess in this pt. is infection with amoeba leading to amoebic liver abscess.
2) How do you approach this patient ?
ANS:
As mentioned earlier in practice we treat both pyogenic and amoebic liver abcess empirically.
* So we cover both bacterial causes with broad spectrum antibiotics and also amoebic causes mostly with metronidazole.
* Next we administer patient with analgesic and antipyretic such as tab.dolo 650mg & tab.Ultracet , to relieve pain and fever.
##Abcess may get ruptured if untreated and cause peritonitis and shock.
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
ANS:
we treat both pyogenic and amoebic liver abcess empirically beacuse we cant differentiate whether the abcess is because of bacterial infection or amoebic infecation.
So we cover both bacterial causes with broad spectrum antibiotics and also amoebic causes mostly with metronidazole.
4) Is there a way to confirm the definitive diagnosis in this patient?
ANS:
Based on right hypochondriac and epigastric pain , fever
USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leucocytosis (suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER ABCESS.
* Considering the following factors:
1) Age of the patient (21) - young & gender- male
2) Single abcess,
3) Right lobe involvement,
# The abcess is most likely to be AMOEBIC LIVER ABCESS.
We can also do USG guided aspiration to confirm the definitive diagnosis in this patient and also the stool culture.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS:
3yrs ago - Hypertension was diagnosed
10days ago- Fever with chills and rigor
4days ago- facial puffiness and periorbital edema
4 days ago - weakness of right upper and lower limb
2days ago- altered sensorium.
Anatomical localization of the problem is Oral , Nasal and Eye.
Primary etiology: Mucormycosis is any fungal infection caused by fungi in the order Mucorales. Species in the Mucor, Rhizopus, Absidia, and Cunninghamella genera are most often implicated.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS:
itraconazole
Deoxycholate ampB
Inj. Liposomal amphotericin B
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
ANS:
Mucormycosis was present even in the pre-Covid era, but is an opportunistic infection. The fungal infection is caused by a group of molds called mucormycetes. These molds live throughout the environment. Mucormycosis mainly affects people with damaged tissue or decreased immunity.
The incidence of mucormycosis in India is around 14/100,000 population while that in Australia is 0.06/100,000 population. The reason behind this is India's hot humid climate where the spores of mucor survive for a longer time.
When the sugars are not controlled, the increased level of sugar in blood provides acidic media which is a favourable environment for the growth of black fungus. Thus, the reason behind increased black fungus cases now can be attributed to uncontrolled diabetes and the use of drugs, which causes further decrease in immunity like steroids.As covid -19 positive pt. are being given steriods which is decreasing the immunity of body , thereby predisposing covid pt. to infection with black fungus.
) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
Please check out the thesis log here for the example of a blogged master chart https://vamsikrishna1996.blogspot.com/2020/10/thesis.html and please get in touch with Dr Sai Charan PGY1 who is liasing between us and the MRD for this project where we hope this data can allow us to get some clues on predicting the factors driving recovery from covid 19.
COVID-19 MASTER CHART:
https://drive.google.com/file/d/1NDF_xnqpY7fRTyiUAEfbQ3NYT_-AGRvg/view?usp=drivesdk
10) Medical Education: (10 marks)